We need to build GP-led chronic disease clinics quickly! These clinics are the missing part of our health system infrastructure leading to hospital system overload made most visible by ramped ambulances.
The solution to hospital overload is not to be found in the hospital. It is to be found by actively supporting patients with complex chronic disease to stay as well as possible and to avoid preventable exacerbations. For this to happen we need to be building integrated complex care clinics staffed by GP-led multidisciplinary teams. This will be a scramble but we have no choice if we want to stop our hospitals descending further into the chaos caused by patient gridlock! Tipping in more and more resources into our hospitals is just not going to work. Forget it!
Change is the price of the survival of our health system!
Australians are living longer but we are carrying a higher burden of complex chronic illness, and our health system is clearly no longer fit-for-purpose. While this reality is generally accepted, successive Governments have failed to enact the necessary policy and infrastructure reforms, and our health system is grinding to a halt as a result.
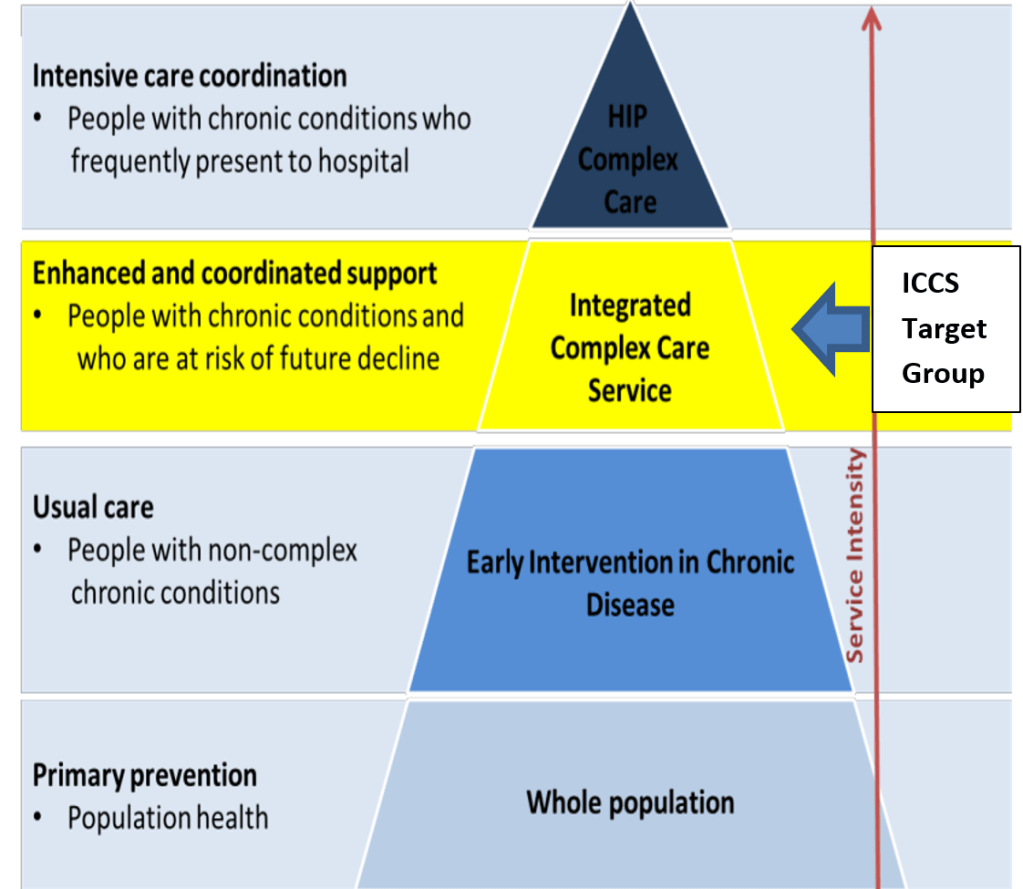
It is entirely a separate article to explore why reform has proven so difficult, so this article will focus on how Integrated Complex Care Service (ICCS) clinics, once established at sufficient scale, will relieve hospital pressure while improving the health of those most at need- those with emergent multi-morbid chronic conditions.
The new Urgent Care Clinics will provide temporary relief for hospital congestion but they will do this at the cost of even more hospitalisations in future as they degrade the capacity of General Practitioners to do what we most need them to do – help people stay well and out of hospital. Urgent Care Clinics provide short-term symptomatic relief for our ailing health system while making things worse for the future. GPs are our chronic disease specialists, and we can’t afford to pretend that they are Emergency Department doctors. That having been said, some ICCS clinics could be contracted to provide urgent care interventions for their enrolled patients.
About the Integrated Complex Care Service Clinics- ICCS as a new ‘system of care’ involves purpose-designed, GP-led clinics that serve as ‘healthcare homes’ for those patients assessed to be at risk of emergent disease-difficult multiple chronic conditions such as heart disease, diabetes, respiratory disease, etc. This is the ‘cocktail’ of conditions that if poorly managed will invariably see people frequently in ambulances seeking hospital admission after acute but usually preventable exacerbations. GPs are specifically trained to help patients manage their chronic illnesses but the prevailing funding, staffing and clinic infrastructure are geared to short consultations totally unsuited to disease-difficult patients. That’s why we need a new system of chronic disease with purpose-designed clinics, and without them hospital collapse is inevitable. More GPs operating under the current service model won’t fix the problem either. We need GPs, working at the ‘top of their clinical license’ supported by multidisciplinary teams working in purpose designed clinics. ’Bolting-on’ new service models onto old infrastructure with outmoded models of care has never worked! It’s time for something completely new.
ICCS Vision- ICCS is a regionally appropriate interdisciplinary ‘system of chronic disease care’ which ensures that every member of the community with complex care needs receives ‘wrap-around’ integrated services as a matter of course. Such Integration will simultaneously build the capacity of general practice and the broader service system while purposefully reducing overall health costs through avoidance of unnecessary hospital admissions, ED presentations and outpatient visits. ICCS will serve to decongest unnecessarily overloaded hospital and associated acute care services. ICCS will stop ambulance ramping progressively.
Purpose – Integrated Complex Care Services (ICCS) seek to improve the experiences and outcomes for people with complex chronic conditions while purposefully reducing overall health system costs, and decongesting hospitals.
The ICCS Target Group -these are people with complex multiple conditions at risk of imminent decline. Patients will be risk-stratified using evidence-based algorithms, and will receive tailored supports delivered by a GP-led multidisciplinary team purposefully interfaced with community-facing General Physician clinics in public hospitals. ICCS patients, especially those with more severe illness and carrying higher-risk, will be under ‘shared and anticipatory care arrangements’ involving ICCS clinics and assigned hospital specialist teams.
ICCS Goals
- Provides coordinated, proactive, responsive, planned and holistic care to people with complex chronic conditions in order to improve their quality of life, reduce their burden of treatment, and slow the rate of clinical and functional decline.
- Empower patients to self-manage, reduce chronic condition risk factors, and optimise their own health and wellbeing.
- Optimises the use of increasingly scarce health system resources through purposeful alignment and integration of service components.
- Empowers affiliating General Practitioners to utilise their chronic condition management skills to manage the full scope of chronic conditions
ICCS overview- ICCS intervenes before people experience decline : provides long-termsupport to patients : involves both care planning and care co-ordination : gives patients access to a hospital general physician-led interdisciplinary chronic condition clinic to deal with acute exacerbations : overcomes institutional and professional silos : ensures shared accountability for outcomes and defines clear expectations of performance : facilitates upgrading of chronic condition management infrastructure and capacity within general practice : purposefully enhances communication and information exchange through standardising eHealth platforms between affiliating providers : rewards those providers doing the heavy-lifting for the most complex patients
Expected benefits of ICCS- ICCS improves patient & carer experience: improves clinical outcomes for enrolled patients: improves healthcare provider experience: reduces acute care service use: improves capacity of general practice to manage complex conditions: reduces overall health costs
Why ICCS? a fair and financially sustainable health system means that we need to modernise care arrangements for the increasing numbers of people carrying the burden of complex chronic illness. ICCS can also have a role in remotely supporting rural hospitals!
Change is the price of the survival of our health system, and it will take a lot of hard work to establish these ICCS clinics. Feathers will be ruffled as some establishment interests will be threatened. It’s our choice now whether to solve ambulance ramping and hospital congestion, or to allow it to descend further into chaos.
For a copy of the ICCS service specification including financial modelling please email – Lawrie.Donaldson@bigpond.com


You must be logged in to post a comment.